Dr. Bharat S Mody Read More.
MS(Orth), MCh (Orth) (Liverpool)
ODTS (RCSE) (London)
AO Fellow (Harvard Univ.) (U.S.A.)
Director & Chief Arthroplasty Surgeon
Dr. Mody is the founder of the hospital. He is also the Head of the Department of Orthopaedics. He is a world renowned orthopaedic surgeon with specialization in Hip, Knee, Arthroscopic surgeries. His team comprises other highly experienced orthopaedic surgeons who are capable of tackling all other aspects of Orthopaedics.Dr. Mody has to his personal credit, an experience of having performed more than 40,000 orthopaedic operations.
Dr. Kshitij Mody
MS (Orth)
Fellowship in Arthroplasty (New York, USA)
Consultant Orthopaedic Surgeon
Dr Kshitij Mody has been described as one of the youngest joint replacement & arthroscopy surgeons in the country to have independently performed over 50 joint replacement surgeries and more than a 100 arthroscopy surgeries after having completed his higher training from Pune and New York. Following his father’s footsteps, he is the next generation consultant orthopaedic surgeon at Welcare Hospital. He specialises in Arthroplasty & Arthroscopy Surgery of the Knee, Hip and Shoulder joints and has become an integral part of the team. He also brings with him youthful energy along with abundant new ideas in the form of advanced technology used at Welcare Hospital.
INTRODUCTION
Tremendous advances have been made in orthopaedic surgery since its inception over 250 years ago. Subspecialties such as Joint Replacement surgery, Arthroscopy, Spinal surgery, hand surgery and other such areas have made significant technological and biological advances in the past 40 years. These have developed into full fledged expertise areas in their own right, and deserve separate departments. Welcare Hospital has therefore established the following departments in Orthopaedics :
ARTHROSCOPY
Perhaps one of the most significant advances to occur in orthopaedic surgery has been the addition of arthroscopic surgery, a minimally invasive technique. Prior to the introduction of endoscopic techniques, large incisions had to be made in order to obtain the surgical exposure needed to treat problems. As a result of the surgical exposure, postoperative, and occasionally persistent, morbidity was common. Surgeons and their patients were forced to weigh the possible benefits of proposed elective surgery against the damage inflicted by the procedure. It was not uncommon that elective surgeries were performed as a last resort, after being postponed until symptoms were either sufficiently great or persistently present to warrant operating. With the introduction of endoscopic techniques came the ability to diagnose problems and even treat them without the subsequent morbidity that had accompanied many prior procedures. Recuperative time was greatly reduced. Because problems were frequently addressed at an earlier stage before the pathology had a chance to advance, results of operations were more likely to be successful.
Arthroscopic surgery has revolutionized the approach to and treatment of joint disorders. Today, arthroscopy is performed on virtually all major joints of the body, and, because of its applications, the world has gained a greater understanding of joint mechanics, anatomy, and function. Its use continues to serve a vital role in the diagnosis and treatment of musculoskeletal ailments because of its high degree of clinical accuracy, low morbidity, infrequent complications, and quick recovery time. Additionally, the development and increased use of arthroscopic techniques have played major roles in the ability to perform surgical procedures on an outpatient basis, thereby saving money and resources.
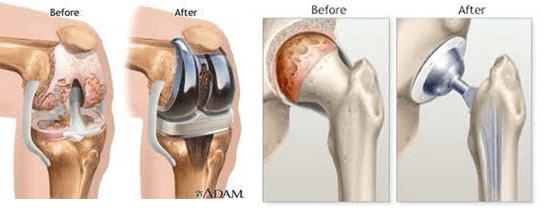
JOINT REPLACEMENT
Before the advent of total joint arthroplasty, patients with significant arthritis of the hip or knee were often forced to endure their pain, with only minimal relief obtained by analgesic medications and other conservative treatments.
Total joint arthroplasties of the hip and the knee have been received with much enthusiasm by the orthopaedic community because of their ability to relieve pain and restore function. The ideas and techniques initiated by the pioneers of joint replacement have given orthopaedic surgeons the power to improve patients’ lives irrevocably and have forever changed the surgical treatment of arthritic joints.
Today, total joint arthroplasties of the hip and the knee are among the most successful surgical procedures performed by any specialty, with marked relief of pain and improved joint function in the majority of patients treated. Total joint arthroplasty is a cost-effective procedure that significantly improves a patient’s quality of life and mobility.
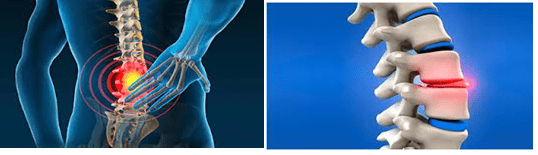
SPINE SURGERY
Spinal surgery has also seen great improvements recently. Minimally invasive disc surgery and enhanced spinal fusions for degenerative disorders are significant advances. Spinal instrumentation, i.e., implantable devices used in the surgical treatment of spinal disorders, has been developed and can significantly correct spinal deformities that were previously untreatable. Likewise, rigid spinal fixation by the pedicle screw and other devices and advances in the techniques of vertebrectomy have improved the treatment of cancer patients with spinal metastases or patients with infection. Often, these treatments can result in significant pain relief and neurological recovery.
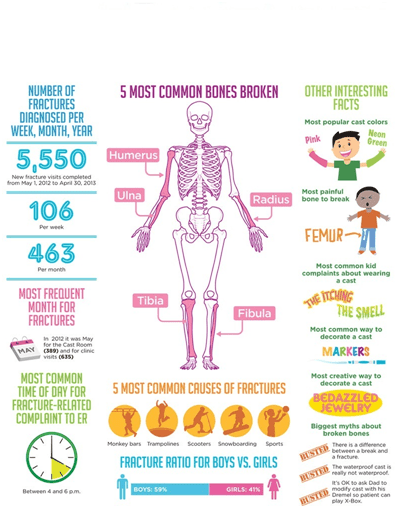
FRACTURE SURGERY
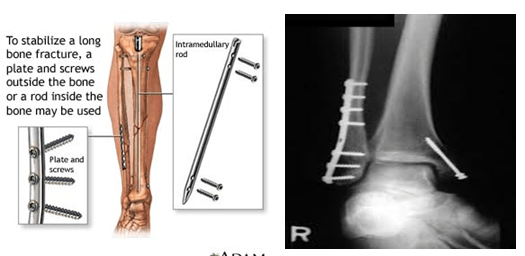
Improved fracture management: open reduction and internal fixation
During the past few decades, there have been significant advances in the way orthopaedists treat fractures. Consequently, fractures are now healing more dependably and with less residual deformity than ever before. Patients treated for orthopaedic trauma are more likely to subsequently lead normal lives without significant disability.
One of the initial accomplishments of the AO/ASIF was the conception of 4 treatment principles that are still valid today. The first principle stresses the importance of obtaining an anatomical reduction of the fracture fragments, especially when the fracture extends into the joint . If closed methods of reduction prove inadequate, open reduction of the fragments by surgical means is carried out. Anatomic reduction is desired to prevent the development of posttraumatic arthrosis and to improve the chances of having a long-lasting and fully functional joint.
The second principle is an extension of the first. After obtaining a good reduction of the fracture fragments, it is necessary to achieve stable fixation of the fragments to maintain the proper anatomic shape. This can be accomplished by a variety of methods ranging from external splints, such as plaster fixation, to internal fixation by plates, screws, wires, and intramedullary nails. Also included are transcutaneous splints—the so-called external fixators . Success of the modern fixation techniques over the past several decades has spawned substantial interest by equipment and instrument manufacturers to develop fracture stabilization equipment.
The third principle is an important concept that has been increasingly recognized as a critical element for proper fracture healing. The preservation of the blood supply to the bone fragments and the soft tissue by means of atraumatic surgical techniques is vital in maintaining adequate nutrition to the fragments and preventing bone necrosis . Understanding of this simple concept is due in large part to the greater efforts of basic science researchers directed at the study of osteosynthesis.
The fourth principle, early and pain-free mobilization, emphasizes the desire for early postoperative motion of the muscles and joints adjacent to the fracture. This concept was contrary to the opinion of the time—that prolonged immobilization was necessary for proper fracture healing to occur. The primary reason for advocating early, protected mobilization is that early motion prevents many of the undesirable sequelae that had, at that time, been accepted as unavoidable with the treatment of fractures. Problems, such as stiff joints, marked muscle atrophy, and osteoporosis, were common following immobilization, and more troublesome complications, such as pneumonia, decubitus ulceration, and deep vein thrombosis, were due in large part to prolonged recumbency. The move from an era in which prolonged immobilization was the mainstay of treatment to today’s emphasis on early motion and rehabilitation has improved, without compromise, fracture healing and posttraumatic musculoskeletal function.
OTHER ADVANCES
The major advances discussed above, i.e., arthroscopic surgery, joint replacement, and open reduction and internal fixation of fractures, have revolutionized the practice of orthopaedic surgery as a whole, but by no means do we intend to imply that the list is comprehensive or that it represents the extent of improvement and development that has occurred in recent times. Indeed, great advances have been made within all the subspecialty areas of orthopaedics.
SPORTS MEDICINE
Sports medicine has recently made great strides in the treatment of shoulder and knee pathology. An improved understanding of shoulder and knee mechanics has led to treatment strategies that are more likely to result in return of the athlete to sports.Procedures such as capsular shrinkage to stabilize the shoulder and arthroscopic reconstruction of the anterior cruciate ligament and partial meniscectomy in the knee are achieving this goal and hopefully resulting in long-term preservation of joint function.
HAND SURGERY
The subspecialty of hand surgery has acquired a valuable tool with the development of microsurgical techniques to perform technically challenging procedures such as nerve and small-vessel repair. Truly remarkable is the ability of surgeons, with the aid of an operating microscope, to reimplant a patient’s severed hand or arm with good recovery of limb function.
PAEDIATRIC ORTHOPAEDIC SURGERY
In paediatric orthopaedics, one of the major areas of progress has been the greatly improved treatments now available for patients diagnosed with malignant bone tumors. These treatments have resulted in the increased survival of many patients whose diagnoses previously carried grave prognoses. Defects created by tumor resection are treated more effectively as well. Techniques such as distraction osteogenesis and bone transport now are used in the reconstruction of these bone defects and in cases in which significant trauma or infection has resulted in deformity. These relatively new technologies, originally used to correct limb length discrepancies in children, can dramatically correct limb deformity and restore function (10).
Today, orthopaedic researchers strive to improve orthopaedic treatment modalities through better understanding of the composition, structure, and function of musculoskeletal tissues (2). Much knowledge has been gained in the past few decades regarding disease processes, such as rheumatoid and degenerative arthritis, and the body’s response to injury. Additionally, the areas of biomechanics and biomaterials have helped create the implants and prostheses that are now an integral part of orthopaedic surgery. Research will continue at a never-before-seen pace and will certainly improve the understanding and treatment of musculoskeletal problems.
Finally, it would be wrong for medical specialists today, especially orthopaedists, not to mention the contribution of diagnostic radiology in regard to diagnostic decision making. Computed tomography and magnetic resonance imaging have found a niche in orthopaedics and are likely to remain as useful diagnostic tools.
COMMON SHOULDER CONDITIONS AND HOW TO TREAT THEM
Welcare Hospital prides itself on providing world class treatment to patients with shoulder injuries, among other musculoskeletal problems. The hospital boasts of a zero percent infection rate postoperatively and has been consistent in providing solutions for shoulder related problems among various other orthopaedic issues.
Welcare hospital is equipped with state-of-the-art facilities which provide for a smooth experience for patients undergoing arthroscopic procedures. Here are some frequently asked questions about shoulder injuries and their management –
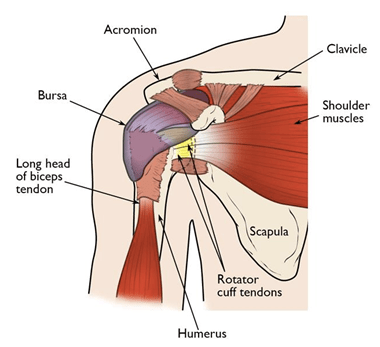
What makes a shoulder joint?
Anatomically, the shoulder joint is made of the arm bone (the humerus), the collar bone (the clavicle) and the shoulder blade (scapula), along with muscles, ligaments and tendons. The joint itself is a ball and socket joint, which means that it helps the arm move in all the directions so any injury to the shoulder leads to a substantial limitation of day-to-day activity.
What are the different shoulder injuries?
Shoulder joint is prone to a number of injuries, the most common of them being Rotator Cuff tears and Frozen Shoulder. Other conditions like Rotator Cuff tendinitis, Shoulder Dislocation and Shoulder Arthritis are also seen.
What is a Rotator Cuff tear?
Rotator cuff is a group of four muscles that come together as tendons to form a covering around the head of the humerus. It attaches the humerus to the shoulder blade and helps to lift and rotate the arm.
When one or more of the rotator cuff tendons is torn, the tendon(s) no longer fully attaches to the head of the humerus therefore destabilising the joint.
Who is at the highest risk for Rotator Cuff tears?
Any action that puts strain on the shoulder joint like lifting heavy objects or falling on an outstretched hand can lead to a rotator cuff tear, which first begins as fraying of the tendons (known as a partial tear) and then to complete tear involving the muscle itself, if the strain is not removed or is repetitive.
Athletes are especially vulnerable to overuse tears, particularly tennis players and baseball pitchers. Painters, carpenters, and others who do overhead work also have a greater chance for tears.
The tear can also occur as a side effect of a shoulder dislocation or of fracture of the collarbone, or as a consequence of ageing since, with age, the blood supply to the cuff tends to decrease which impairs the ability of the muscles and tendons to repair themselves. Rarely, the tear could occur due to bone overgrowth, known as a bony spur, on the underside of the acromion bone. The bony spur impinges on the muscles and injures them every time the arm moves.
What are the symptoms of a Rotator Cuff tear?
If the tear is sudden, like due to a fall on an outstretched hand, it causes intense pain in the shoulder and inability to move the arm at all. If the tear is gradual, the first symptoms would be mild pain on lifting the arm over the head. Over time, the pain becomes worse, often occurring even at night and the arm movements become heavily restricted.
How can a Rotator Cuff tear be treated?
As a rotator cuff tear could be anywhere from mild to severe, patients are initially asked to take ample rest and analgesics (anti-pain medications). If the pain persists, steroid injections may be given. In cases where the tear is large or the blood supply is inefficient, a shoulder surgery is done to repair the injury. Surgery is also done if the injury has failed to heal after 12 months of trauma, or if the injury is a recent, acute one.
What is a Frozen Shoulder?
Another very common condition affecting the shoulder is Adhesive Capsulitis, usually called the Frozen Shoulder.
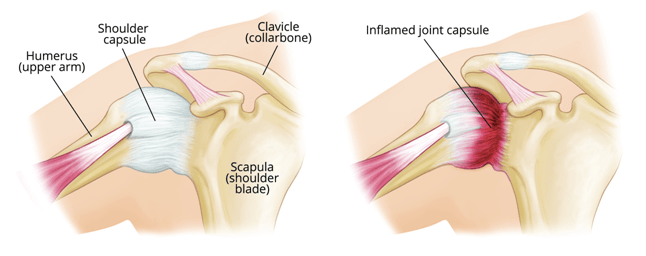
It is the inflammation of the capsule of the shoulder joint seen in people with diabetes, hypothyroidism, hyperthyroidism, Parkinson’s disease, and cardiac disease. It is also sometimes seen after a period of immobilisation following any shoulder surgery and can be prevented by starting physiotherapy of the shoulder as soon as possible, postoperatively.
How can a Frozen Shoulder be treated?
Since the most marked initial symptom is pain, treatment here also involves rest and analgesics followed by physiotherapy to regain the shoulder movements. A procedure known as hydrodilation, in which sterile fluid is injected in the shoulder joint to stretch the capsule, may be done when non-surgical methods fail. In severe cases surgery is preferred.
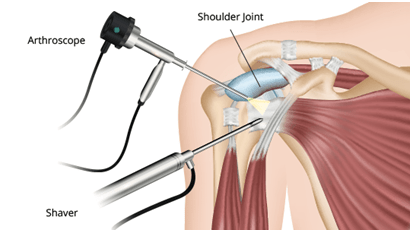
What is Shoulder Arthroscopy?
Diving deeper regarding the surgical options for shoulder injuries, Shoulder Arthroscopy has now replaced the conventional open surgery for almost all shoulder related procedures. Previously, open repair was the treatment of choice but it led to a high prevalence of infections and anaesthetic complications, along with postoperative stiffness in the joint and a long hospital stay.
Regarding an arthroscopic surgery, the patient is kept in the hospital for an hour or two postoperatively and then discharged, effectively making it an outpatient procedure and hence, the procedure of choice.
In Shoulder Arthroscopy a small camera, known as the arthroscope, is inserted into the shoulder joint and images are displayed on a television screen to guide the surgeon as to where to operate.
Since the instruments used in this procedure are thin and small, very tiny incisions are required, as opposed to big incisions in open repair.
On discharge, the patient is taught how to support his shoulder with a sling, and rest and analgesics are advised.
Shoulder arthroscopy has also successfully, and commonly, been used for bone spur (bone overgrowth) removal, repair of ligaments, removal of inflamed tissue or loose cartilage and repair for recurrent shoulder dislocation.
Platelet-Rich Plasma (PRP)
During the past several years, much has been written about a preparation called platelet-rich plasma (PRP) and its potential effectiveness in the treatment of injuries.
Many famous athletes — Tiger Woods, tennis star Rafael Nadal, and several others — have received PRP for various problems, such as sprained knees and chronic tendon injuries. These types of conditions have typically been treated with medications, physical therapy, or even surgery. Some athletes have credited PRP with their being able to return more quickly to competition.
Even though PRP has received extensive publicity, there are still lingering questions about it, such as:
What Is Platelet-rich Plasma (PRP)?
Although blood is mainly a liquid (called plasma), it also contains small solid components (red cells, white cells, and platelets.) The platelets are best known for their importance in clotting blood. However, platelets also contain hundreds of proteins called growth factors which are very important in the healing of injuries.
PRP is plasma with many more platelets than what is typically found in blood. The concentration of platelets — and, thereby, the concentration of growth factors — can be 5 to 10 times greater (or richer) than usual.
To develop a PRP preparation, blood must first be drawn from a patient. The platelets are separated from other blood cells and their concentration is increased during a process called centrifugation. Then the increased concentration of platelets is combined with the remaining blood.
How Does PRP Work?
Although it is not exactly clear how PRP works, laboratory studies have shown that the increased concentration of growth factors in PRP can potentially speed up the healing process.
To speed healing, the injury site is treated with the PRP preparation. This can be done in one of two ways:
- PRP can be carefully injected into the injured area. For example, in Achilles tendonitis, a condition commonly seen in runners and tennis players, the heel cord can become swollen, inflamed, and painful. A mixture of PRP and local anesthetic can be injected directly into this inflamed tissue. Afterwards, the pain at the area of injection may actually increase for the first week or two, and it may be several weeks before the patient feels a beneficial effect.
- PRP may also be used to improve healing after surgery for some injuries. For example, an athlete with a completely torn heel cord may require surgery to repair the tendon. Healing of the torn tendon can possibly be improved by treating the injured area with PRP during surgery. This is done by preparing the PRP in a special way that allows it to actually be stitched into torn tissues
What Conditions are Treated with PRP? Is It Effective?
Research studies are currently being conducted to evaluate the effectiveness of PRP treatment. At this time, the results of these studies are inconclusive because the effectiveness of PRP therapy can vary. Factors that can influence the effectiveness of PRP treatment include:
- The area of the body being treated
- The overall health of the patient
- Whether the injury is acute (such as from a fall) or chronic (an injury developing over time)
- Chronic Tendon Injuries
- According to the research studies currently reported, PRP is most effective in the treatment of chronic tendon injuries, especially tennis elbow, a very common injury of the tendons on the outside of the elbow.
- An injection of PRP is used to treat tennis elbow.
The use of PRP for other chronic tendon injuries — such as chronic Achilles tendonitis or inflammation of the patellar tendon at the knee (jumper’s knee) is promising. However, it is difficult to say at this time that PRP therapy is any more effective than traditional treatment of these problems. - Acute Ligament and Muscle Injuries
- Much of the publicity PRP therapy has received has been about the treatment of acute sports injuries, such as ligament and muscle injuries. PRP has been used to treat professional athletes with common sports injuries like pulled hamstring muscles in the thigh and knee sprains. There is no definitive scientific evidence, however, that PRP therapy actually improves the healing process in these types of injuries.
- Surgery
- More recently, PRP has been used during certain types of surgery to help tissues heal. It was first thought to be beneficial in shoulder surgery to repair torn rotator cuff tendons. However, the results so far show little or no benefit when PRP is used in these types of surgical procedures.
Surgery to repair torn knee ligaments, especially the anterior cruciate ligament (ACL) is another area where PRP has been applied. At this time, there appears to be little or no benefit from using PRP in this instance. - Knee Arthritis
- Some initial research is being done to evaluate the effectiveness of PRP in the treatment of the arthritic knee. It is still too soon to determine if this form of treatment will be any more effective than current treatment methods.
- Fractures
- PRP has been used in a very limited way to speed the healing of broken bones. So far, it has shown no significant benefit.
- Conclusion
- Treatment with PRP could hold promise, however, current research studies to back up the claims in the media are lacking. Although PRP does appear to be effective in the treatment of chronic tendon injuries about the elbow, the medical community needs more scientific evidence before it can determine whether PRP therapy is truly effective in other conditions.
- Even though the success of PRP therapy is still questionable, the risks associated with it are minimal: There may be increased pain at the injection site, but the incidence of other problems — infection, tissue damage, nerve injuries — appears to be no different from that associated with cortisone injections.
- If you are considering treatment with PRP, be sure to check your eligibility with your health insurance carrier. Few insurance plans, including workers’ compensation plans, provide even partial reimbursement.